Alzheimer’s disease remains a formidable adversary in the realm of health care, casting a long shadow over millions of lives. The recent advancements in medication aimed at battling this insidious condition have been considerable, yet one glaring problem persists: a shocking discrepancy in how these drugs affect men and women. A closer inspection of clinical data suggests that while groundbreaking treatments like lecanemab may indeed add a few precious years of independence for patients, this boon may be reserved disproportionately for male patients. As we delve deeper into these findings, the implications become not just a matter of scientific curiosity but also societal urgency.
An Uneven Playing Field
Lecanemab, touted as a revolutionary drug approved by the FDA, offers a 27 percent reduction in cognitive decline over an 18-month trial compared to a placebo. However, this statistic masks a troubling reality: female participants experienced only a 12 percent reduction, revealing a staggering 31 percent difference in effectiveness when compared to their male counterparts. Neuroscientist Daniel Andrews and his team highlighted this lavished promise intertwined with the unsettling truth—two-thirds of Alzheimer’s patients are women, and yet they may not gain the same benefits from this therapy.
The issue expands beyond mere statistical averages; it shines a light on a system that has undervalued the treatment responses of women. The shocking reality is that clinical trials have historically favored male participants to the detriment of female-specific outcomes. Andrews suggests this is not a mere oversight but a deep-seated neglect that echoes the broader societal tendency to discount women’s health issues. This kind of research inequality may undermine confidence in a system charged with the responsibility of safeguarding the health of all individuals.
The Flawed System of Clinical Trials
The findings are a rallying cry for the reform of clinical trial methodologies. In the past, the absence of sufficient female representation raised serious concerns, even within the scientific community. As highlighted by researchers like Marina Lynch, the consistent lack of effort to stratify clinical data by sex has led to a plethora of oversights. The dire need for a more equitable approach cannot be overstated. Until we prioritize the differences in drug response based on sex, we risk perpetuating an inequitable healthcare landscape that favors the norms and biology of men over women.
Moreover, while the study’s authors express reservations about declaring lecanemab ineffective for women, there is an unsettling possibility that the very biology of the drug may favor male biology. This suspicion illuminates complexities not just in Alzheimer’s treatment but also in how we perceive and approach health care. If the prevailing wisdom remains blind to these differences, we will remain stalemated in our fight against diseases that discriminate based on gender.
The Implications of Amyloid Targeting
Lecanemab’s primary action, targeting amyloid plaques, has long been regarded as a leading mechanism behind Alzheimer’s disease. However, fresh perspectives from research indicate that these protein clumps may not be the unequivocal villains we once believed them to be. This nuanced understanding reveals another layer of complexity in treatment efficacy: some patients who meet the clinical criteria for Alzheimer’s may not even have significant amyloid buildup at the point of diagnosis. What does this mean for women, and what’s left unexamined in this sweeping narrative of amyloid targeting?
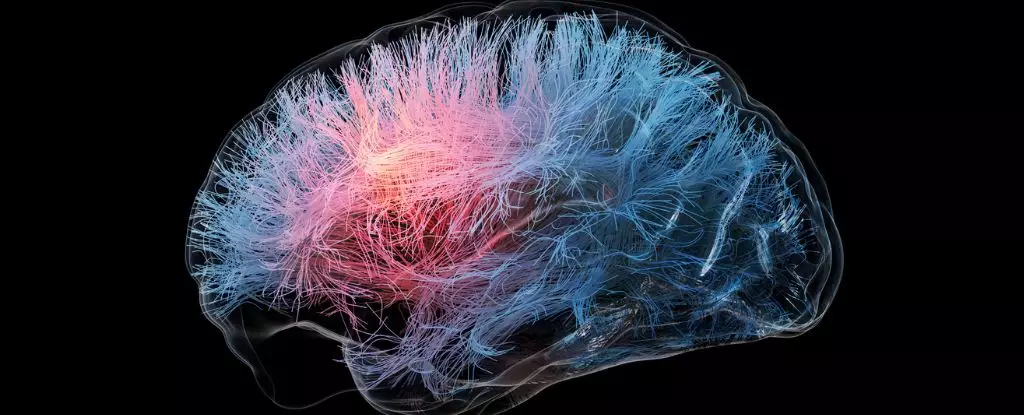
The suggestion that hormonal differences and sex-linked genetic factors may affect how our brains age, and respond to treatments gives rise to a whole new chapter in neurological research. It challenges drug developers to rethink their research focus and merge insights from both male and female brain studies. The future of effective treatment lies not in a gender-neutral approach but in acknowledging gender as a critical variable.
Addressing the Gender Bias in Neuroscience
The significance of the findings cannot be overstated, particularly in light of the substantial gender biases observed within neuroscience. In 2019, a mere 5 percent of neuroscience studies examined the role of sex, revealing a stunning blind spot in a field where understanding brain aging is of paramount importance. The admonishment from a coalition of international scientists underscores a painful truth: neglecting the nuances of gender in research only compounds the burden of diseases like Alzheimer’s on women.
As the wave of new treatments continues to roll out, we must remain vigilant against complacency. There is an urgent need for more nuanced clinical trial designs that do not merely include females for the sake of diversity but critically analyze their performance against all parameters, including sex. Until we dismantle the biases entrenched in how we study and treat diseases like Alzheimer’s, we are relinquishing our collective responsibility to secure health equity for all.

Leave a Reply