In recent times, the narrative surrounding the NHS has painted a picture of cautious optimism, often masking the profound vulnerabilities lurking beneath the surface. Politicians and officials tout multi-year plans and strategic reforms as evidence of a resilient health service. Yet, beneath this veneer lies a fragile ecosystem plagued by chronic underfunding, staff dissatisfaction, and mounting public skepticism. The current situation—marked by ongoing strikes and failed negotiations—exposes the illusion that the NHS can be fixed solely through political will or bureaucratic tinkering. The truth is, the core issues remain unaddressed, threatening the very foundation of Britain’s cherished healthcare system.
The Illusive Promise of a Long-Term Reform Strategy
A decade-long reform plan sounds ambitious and forward-thinking, but it often serves as a distraction from dealing with immediate crises. Such comprehensive strategies tend to be overly optimistic and disconnected from on-the-ground realities. The assumption that workforce goodwill will sustain reforms is dangerously naive; it essentially banks on staff generosity without offering sustainable compensation or working conditions. When the backbone of the NHS—its doctors, nurses, and social care workers—feels undervalued and underpaid for years, no long-term plan can succeed without urgent, meaningful investment. Yet, governments continue to prioritize grand visions over tangible, immediate support for healthcare staff, thus risking further deterioration of service quality.
The Myth of Negotiation and Goodwill
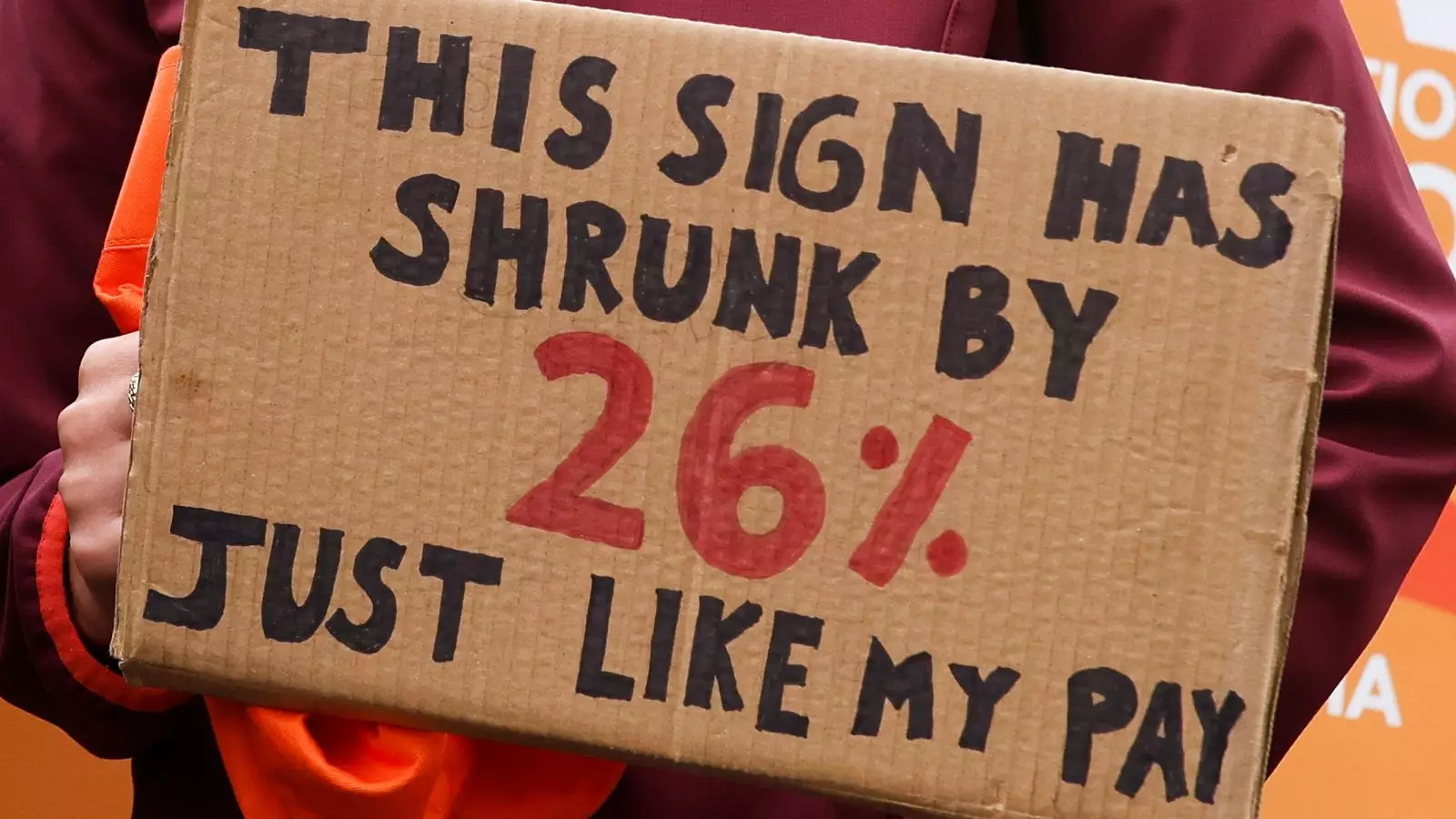
The recent negotiations between the health secretary and the British Medical Association reveal a fundamental misjudgment. While officials frame their efforts as attempts to protect patient care, the reality is a tangled web of political posturing and economic stretch. The claim that the government has already given a near-30% total pay rise is a misleading oversimplification. This figure ignores inflation, increased workloads, and years of stagnation that have left staff feeling undercompensated. Moreover, the notion that “local trust leaders” will be able to make better decisions sounds promising but is ultimately a superficial solution that sidesteps the systemic issues of funding and workforce planning. Without addressing root causes, these localized measures merely serve as sticking plasters on a bleeding wound.
The Toxic Politics of Blame and Misinformation
The escalation of rhetoric between political figures and unions reveals how deeply entrenched the problem has become. Each side blames the other for risking patient safety, fostering a climate of distrust and polarization. Politicians like Wes Streeting emphasize local decision-making as a way to mitigate harm, but this approach risks fragmenting what should be a unified health service. Meanwhile, unions argue that without proper pay and safety measures, patient care is compromised. This blame game ignores the uncomfortable truth: both sides are entrenched in a cycle of mistrust, and neither is willing to make the substantial sacrifices needed to overhaul a system that is fundamentally broken. The populist language and finger-pointing only distract from the urgent need for honest governance and genuine investment.
The Human Cost of Political Stagnation
At its core, the NHS crisis is a human tragedy, not just a policy conundrum. Medical professionals dedicate their lives to caring for others, yet they regularly face burnout, underpayment, and the moral injury of working in an overstretched system. The patient experience suffers as a result—appointments canceled, wait times ballooning, and anxieties mounting among those most in need. Politicians’ reluctance to confront the hard truths about funding and staffing leaves frontline workers trapped in a cycle of inadequate support, which in turn jeopardizes patient safety. The promise of reform feels hollow when the real cost is the wellbeing of those who rely on a system that has long been forgotten or neglected at the government’s rhetorical altar.
The grand illusions of progress and reform in Britain’s NHS obscure the fact that meaningful change requires more than political slogans and superficial measures. Until genuine investment is made, and the core issues of pay, staffing, and working conditions are addressed honestly, the service will continue to falter. The current stalemate is not just a political fight—it’s a moral failure to prioritize the wellbeing of both healthcare workers and patients. If Britain cannot muster the courage to tackle these problems head-on, the reputation of the NHS as a universal, compassionate institution will be forever tarnished by its own neglect.

Leave a Reply